Understanding Hysterectomy Procedure Options: A Complete Guide by Expert Obstetricians & Gynecologists

When it comes to women’s health and reproductive wellness, hysterectomy procedures are among the most significant surgical interventions performed by obstetricians and gynecologists. Whether for treating benign conditions, managing complex health issues, or providing relief from chronic symptoms, understanding the different hysterectomy procedure options is essential for making informed decisions. This comprehensive guide will delve into all aspects of hysterectomies, covering surgical techniques, benefits, risks, recovery, and how an expert healthcare team, like that at drseckin.com, can facilitate optimal outcomes.
What is a Hysterectomy?
A hysterectomy is a surgical procedure that involves the removal of the uterus, and in some cases, surrounding tissues and organs. The procedure is performed for various medical reasons, including uterine fibroids, abnormal bleeding, endometriosis, prolapse, or cancer. It is one of the most common gynecologic surgeries worldwide, with millions of women undergoing the procedure annually.
Why Consider a Hysterectomy? Common Indications
- Uterine fibroids: Noncancerous growths causing pain, pressure, or bleeding.
- Heavy or irregular menstrual bleeding: When conservative treatments fail to provide relief.
- Endometriosis: Severe pain and fertility issues associated with endometrial tissue outside the uterus.
- Uterine prolapse: Descent of the uterus into the vaginal canal leading to discomfort.
- Cancer: Malignant or precancerous conditions involving the uterus, cervix, or ovaries.
- Adenomyosis: Growth of endometrial tissue within the uterine muscle, causing pain and enlargement.
Types of Hysterectomy Procedures: Exploring Your Options
Understanding the various hysterectomy procedure options is crucial to choose the most suitable approach tailored to individual health needs, personal preferences, and surgical considerations. The main types of hysterectomies include:
1. Total Hysterectomy
This involves removal of the entire uterus and cervix. It is the most common form and typically indicated for conditions involving both the uterus and cervix. The procedure can be performed through different surgical techniques based on patient factors.
2. Partial or Supracervical Hysterectomy
In this procedure, only the upper part of the uterus is removed, leaving the cervix intact. This option may be preferred to preserve pelvic floor stability or avoid removing the cervix due to specific medical reasons.
3. Radical Hysterectomy
This extensive surgery involves removal of the uterus, surrounding tissues, part of the vaginal canal, and lymph nodes. It is usually performed for cervical or endometrial cancer.
4. Hysterectomy with Salpingo-Oophorectomy
This combines uterus removal with removal of the ovaries and fallopian tubes. It is often recommended for certain cancers or high-risk cases to reduce hormone production and cancer spread.
Minimally Invasive Hysterectomy Techniques
Advances in surgical technology have introduced minimally invasive approaches that offer numerous benefits over traditional open surgery. These techniques include:
1. Laparoscopic Hysterectomy
This involves using a tiny camera (laparoscope) inserted through small incisions in the abdomen. Surgeons perform the removal with specialized instruments, providing less pain, faster recovery, and minimal scarring.
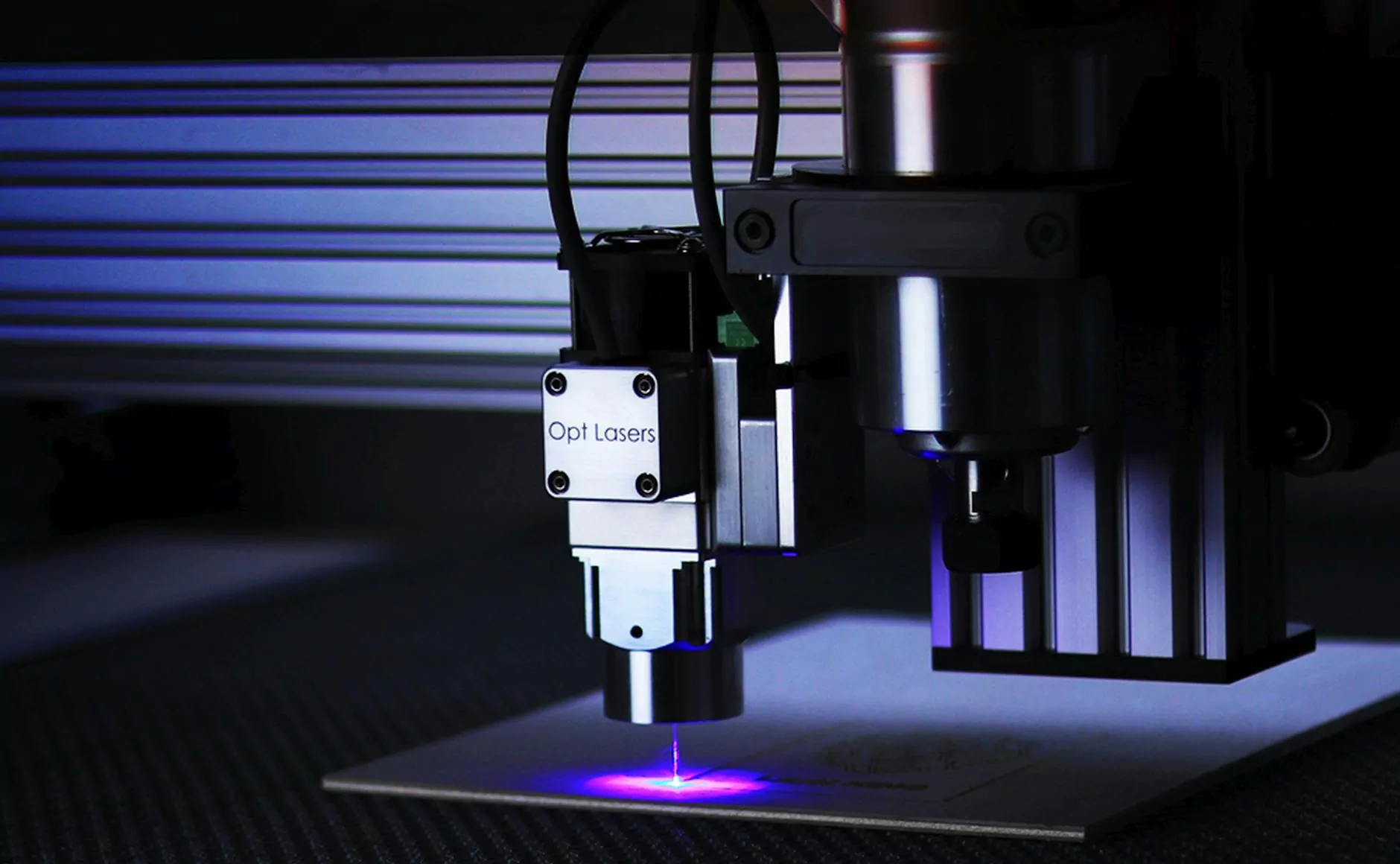
2. Robotic-Assisted Hysterectomy
An advanced form of laparoscopic surgery where robotic systems enhance precision, flexibility, and control. It allows for intricate procedures to be performed with high accuracy.
3. Vaginal Hysterectomy
Performed entirely through the vaginal canal without external incisions, this technique is typically suited for cases where the uterus isn’t enlarged or adherent tissues aren’t present.
4. Abdominal Hysterectomy
Involves a larger incision in the lower abdomen. Though more invasive, it may be necessary for complex cases involving large fibroids, extensive endometriosis, or cancer.
Choosing the Right Hysterectomy Procedure Option
Deciding among the hysterectomy procedure options depends on several factors, including:
- Medical condition: Size and location of fibroids, extent of disease, or cancer stage.
- Overall health and anatomy: Prior abdominal surgeries, pelvic anatomy, and comorbidities.
- Preservation of fertility: Desire to retain reproductive capabilities.
- Recovery considerations: Minimally invasive options generally promote quicker healing.
- Surgeon expertise and available technology: The experience and resources of your healthcare provider.
Benefits of Minimally Invasive Hysterectomy
Choosing minimally invasive hysterectomy procedure options offers numerous advantages:
- Reduced postoperative pain and discomfort.
- Shorter hospital stays and faster return to daily activities.
- Minimal scarring and better cosmetic outcomes.
- Lower risk of infections and complications associated with open surgery.
- Preservation of pelvic support structures when feasible.
Risks and Considerations in Hysterectomy Surgery
While hysterectomy is generally safe, it involves risks that patients should be aware of:
- Bleeding and hemorrhage.
- Infection at incision sites or internally.
- Damage to surrounding organs such as the bladder or bowel.
- Risks related to anesthesia and surgical stress.
- Postoperative hormonal changes if the ovaries are removed.
- Potential impact on sexual function, though most women report no adverse effects when properly managed.
Recovery and Postoperative Care
Recovery time varies based on the procedure type and individual health. Generally, patients can expect:
- Initial rest and limited activity for several days.
- A gradual return to normal activities over 4–6 weeks.
- Follow-up appointments to monitor healing and address concerns.
- Advice on managing symptoms such as pain, fatigue, or vaginal bleeding.
- Long-term lifestyle adjustments if ovaries are removed, including hormone management.
Choosing an Expert Surgical Team: Why Trust Dr. Seckin
Signing up with a skilled obstetrician & gynecologist like Dr. Seckin ensures a tailored, safe, and effective approach to your hysterectomy procedure options. Benefit from:
- Personalized treatment plans based on your unique health profile.
- Access to the latest surgical technologies and minimally invasive techniques.
- Comprehensive preoperative counseling and candid discussions about risks and benefits.
- Dedicated postoperative care for optimal recovery and long-term health.
Visit Dr. Seckin's website to learn more about expert gynecological care and schedule a consultation for your individual needs.
Conclusion: Making Informed Choices about Your Hysterectomy
Choosing the appropriate hysterectomy procedure options involves a detailed understanding of the surgical techniques, benefits, potential risks, and recovery process. Advances in minimally invasive surgery have transformed patient outcomes, offering less pain and quicker recovery times. Collaborate with experienced healthcare providers, like those at drseckin.com, to ensure your treatment aligns with your health goals and lifestyle preferences. Remember, informed decisions empower you to take control of your reproductive health and overall well-being.